Pharmacogenomics can be understood as the science of how genes interact with medication in a person’s body to affect its response. We know that every individual is different and would respond differently when given the same medication. Some may need a higher dose. Some may need medication of a different mechanism. In the past, we are not able to determine who will need what and medication treatment is often a one size fit all or even carpet bombing approach. The lack of predictability to side effects, and effective doses often leave doctors blind sided and frustrated.
Today, we know that our genes play a big part in how our body interacts with drugs. A major system is the cytochrome P-450 (CYP) family of enzymes which metabolizes drugs in the liver. To put it simply, the presence of genetic differences (what we call allelic variants / polymorphisms ) in the CYP enzymes result in three main phenotypes (observable characteristics), i. e. poor metabolizers (PMs), normal metabolizers (NMs), and extensive metabolizers (EMs). This results in some people having more side effects with certain medications and can account for some of the reasons why some people need higher or lower doses of medication.
Using clinical depression as an example, there may be individuals who have major gene-drug interaction. An increase in the metabolism due to the genotype (genes) may decrease the patient’s exposure to the medication, necessitating a higher dose. An inadequate dose may result in treatment failure or mimic treatment resistance. Conversely an decrease in metabolism may increase exposure to medication resulting in more side effects like diarrhoea or nausea.
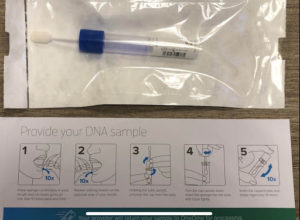 Now that pharmacogenomic testing is available, we can now piece in this missing part of the jigsaw. Testing for certain polymorphisms / genetic differences before prescribing certain drugs can help avoid adverse drug effects and improve efficacy.
Now that pharmacogenomic testing is available, we can now piece in this missing part of the jigsaw. Testing for certain polymorphisms / genetic differences before prescribing certain drugs can help avoid adverse drug effects and improve efficacy.
